What causes acne and acne scarring?

By Ulrik knap, md, laser & acne scar specialist
Treating acne scars is a medical art that requires great skills and the use of the right methods. Not one method fits all acne scar types. Hence, I treat acne scars with different methods and choose the best methods for each individual acne scar. Combining different methods – when relevant – is the only way to achieve the highest cure rate. Therefore, patients come from most of the world to visit my office and have their acne scars treated by me personally.
In this short article, I’ll tell you about acne (in Part 1), and in Part 2, I’ll talk about acne scarring, what it is, what causes acne scarring, why some people develop acne scars and others don’t, and how to treat acne scarring.
Let’s get started….
Part 1: Acne
What causes acne?
Acne is a disease that affects over 90% of all adolescents, typically starting in puberty.
But what is acne?
Basically, there are 4 major recognized steps in developing pimples. These are:
- increased oil production (sebum) in the oil glands
- clogging of the hair follicles
- trapping of certain bacteria and increased bacteria growth around the hair follicle
- inflammation
Okay, so this might need a bit of explanation if you’re new to this subject… so let’s dive into each individual step and discuss what they mean….


Step 1 in acne: Increased oil production
Increased oil production in the oil glands! What does this mean and why does this have anything to do with acne…?
Well, acne is actually a disease that affects the oil glands of the skin. As the name suggests, the oil glands are where the oil in the skin is produced which makes the skin oily and prevents it from drying out.
One of the things which certainly can increase oil production is the sex hormones in the body. That’s why acne gets worse during changes in hormonal levels in pre-teens, and why some women experience acne with hormonal fluctuation during the menstrual cycle and pregnancy.

Step 2 in acne: Clogging of the hair follicle
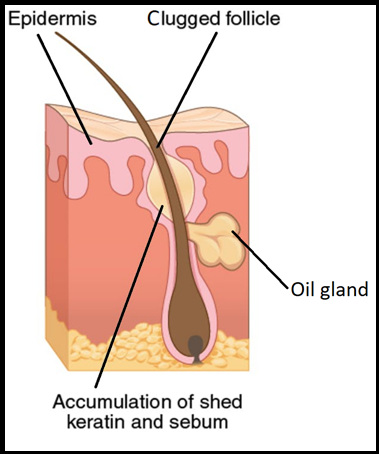
The next step in developing acne is clogging of the hair follicles. The oil glands and hair follicles are actually part of the same structure in the skin, called a pilosebaceous follicle.
This unit is shown in the figure.
When the oil glands (sebaceous glands) and hair follicles become clogged with oil (sebum) and dead skin cells (keratin), whiteheads and blackheads develop.
Having whiteheads and blackheads is the first step towards a red inflamed pimple.
Step 3 in acne: Bacterial growth
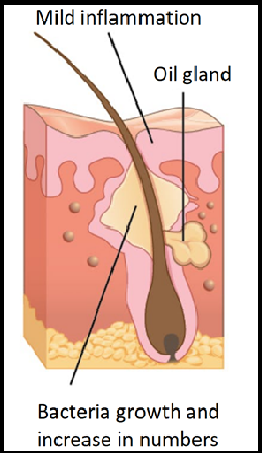
As part of the skin flora present on most healthy adult humans’ skin and deep within follicles and pores, lives a bacteria called Propionibacterium acnes, or P. acnes for short.
When the hair follicle gets clogged, P. acnes gets trapped in the hair follicle together with all the oil from the oil gland.
P. acnes simply loves those warm and oily conditions. This creates optimal conditions for the bacteria to grow. Thus, when P. acnes gets trapped together with all the oil from the oil gland, the bacteria start to multiply and increase rapidly in numbers.
This is illustrated in the figure.
Step 4 in acne: Inflammation
Now, we have examined the first 3 steps in acne. To summarize these steps were: 1) increased oil production, 2) clogging of the hair follicle and 3) bacteria growth of P. acnes.
The last step in the process of developing acne is inflammation.
But what is inflammation, you might ask?
Well, inflammation in this context is the body’s response to the bacterial growth of P. acnes. This response is called an immune response which is how your body recognizes and defends itself against bacteria, viruses, and substances that appear foreign and harmful.
The immune response is generated by the body’s own immune system, which you can perceive as your personal defense team that comes charging to the rescue when substances that appear foreign and harmful invade the body… such as P. acnes.
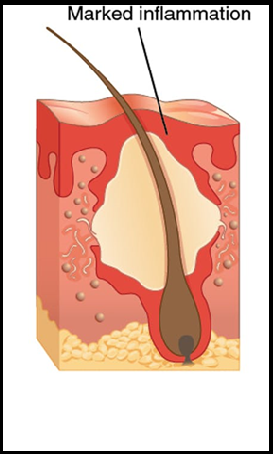
Part of the immune response is inflammation. When inflammation occurs, you get an inflamed, red pimple that hurts when touched.
The commonest affected areas of acne include the face, back, and chest because these areas have a high concentration of oil glands.
Part 2: Acne scars
In Part 1, you learned about the basics of acne. Now, it’s time to dive into the subject concerning acne scarring. You probably have a lot of questions about this subject.
So let’s continue…
What is acne scarring?
As the name suggests, acne scarring is scarring which is caused by acne. The prevalence of acne scarring in the general population is estimated to be 1-11%. Hence, far from everyone with acne develops scarring. However, when acne scars develop, they may be both disfiguring and life-altering causing mental stress, anxiety, and depression.
As a board-certified laser and acne scar specialist, I believe that it’s very important to treat acne scars properly and with the right methods to achieve the highest possible cure rate in favor of my patients.

What are the different Atrophic acne scar types?
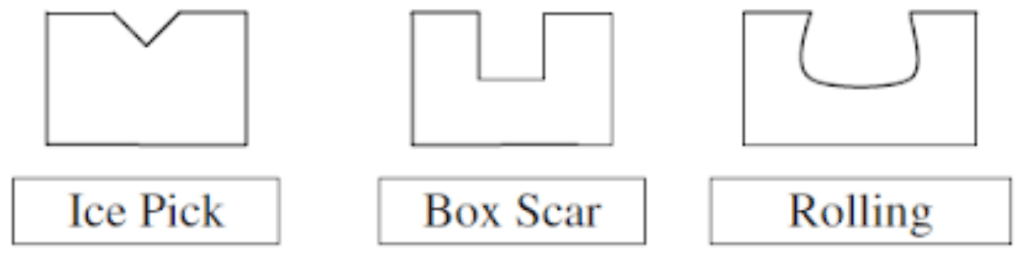
Acne scars can be classified in different acne scar types, including atrophic acne scars, hypertrophic scars, keloids, boxcar scars, ice pick scars, enlarged pores, rolling scars, tethered scars, and anchored scars.
When consulting a patient with acne scars in my practice, firstly I make a thorough skin examination to identify the acne scar type of each individual acne scar.
I use tangential lighting to see the depths of the scars, touch the skin to identify deep fibrosis in the skin, and I have the patient mimic and smile to identify any tethering and anchored acne scars.
Thereafter, I map and photograph the acne scars.
My skin examination is the foundation for planning and tailoring the optimal acne scar revision program for each individual patient.
Please learn more about the different acne scar types and treatments here.
What causes acne scarring?
In Part 1 of this article, you learned about the 4 steps in acne, and you might remember that the fourth step in the process was inflammation.
Inflammation is the feature that makes the pimple get red and sore when touched. It is also the inflammation and the immune response which is how your body recognizes and defends itself against bacteria, including P. acnes which is known to play an important role in acne.
When the bacteria have been defeated, the wound healing begins aiming to repair the damages after the fight between the bacteria and the immune system.
Wound healing is one of the most complex biological processes in the body and involves soluble chemical mediators, extracellular matrix components, fibroblasts, and a lot of different kinds of cells.
Before I get to that part, you should know that the skin (dermis) is made up of both collagen fibers, elastic fibers and a lot of other things which we call the extracellular matrix. This is illustrated in the rather complicated figure below…


The equilibrium of wound healing
The repairing process (wound healing) occurs mainly in the lower layers of the skin (called the dermis) around the hair follicles and oil glands since this is where acne originates. It’s also in this part of the skin that acne scarring occurs.
The repairing process is managed by the immune system, which all at the same time both stimulate the production of new tissue as well as the degradation of tissue which was damaged during the initial fight between the bacteria and the immune system.
Hence, this is an equilibrium between the creation and degradation of tissue, including collagens, elastins, and extracellular matrix.
In patients who are prone to develop acne scarring, there is an imbalance between what is too much and too little!
If the equilibrium is shifted towards too much destruction of collagen fibers, there’s a loss of tissue. That’s what happens in atrophic acne scars which encounter for 80 to 90 % of all acne scars. Less commonly, there is a net gain of collagen that results in hypertrophic or keloid scars.
Moreover, by comparing the immune response in acne lesions in scar-prone and non-scar-prone patients, it appears that the inflammatory reaction around the hair follicle and oil glands is much stronger and lasts longer in patients with scarring compared to patients with acne who do not develop acne scarring.

A lot of things affect how the skin heals after acne. Meanwhile, though the pathogenesis of acne scarring is not completely understood, we at least know some of the features that play a role in developing acne scarring so far.
Why do some develop acne scarring while others don’t?
More than 90 percent of all adolescents develop acne at some point. Some only have a pimple or two, while others might have moderately or severely inflammatory nodulocystic acne that can last for years.
Patients with severe acne are typically more prone to develop acne scars. However, even in mild and moderate cases, scarring occurs now and then.
So, why is that…?
Well, it all comes down to the wound healing. How an individual heals basically depends on the genes.
Hence, it’s the genes that determine the equilibrium between the creation and degradation of tissue during wound healing.
You cannot tell in advance who in their teens develop acne but no scarring, and who on the contrary develop acne scarring or the severity of that scarring. That secret all lies within the genes which are inherited from your parents.


Can all acne scars be treated?
Yes, absolutely. No matter how old or severe an acne scar is, it can always be improved. In my hands, acne scars can on average be improved with 70-80% with a tailored acne scar revision program. This is good news if you have acne scarring.
As a laser and acne scar specialist, I have specialized in treating patients with acne scarring. This is a medical art that requires years of practice and experience.
The key to success is to analyze each individual acne scar, identify the acne scar type and the skin type and thereafter matching the acne scar type with the right method. There are many different acne scar types, including boxcar scars, ice pick scars, rolling scars, tethered scars, and anchored scars. Each acne scar type should be treated individually. The first step in all my acne scar consultations is to identify the acne scar type. This is a 3-dimensional skin examination that requires that I see the acne scars in certain lighting, touch the skin and the scars, as well as have the patient mimic and smile to identify tethering and anchored scars.
When I have done my initial skin and scar analysis, I map and photograph the scars. Finally, I plan an individual acne scar revision program for the patient. This is a tailored program, which depends on the acne scar types, the severity of the scars, as well as the skin type.
The acne scar revision program typically lasts 4-8 months but may last shorter or longer.
I have developed a unique method to treat acne scars which gives a high cure rate. Only by identifying the right acne scar type of each individual acne scar during my initial acne scar analysis, I can match the acne scar with the treatment that gives the highest cure rate of each individual acne scar.
This is why patients with acne scars come from most of the world to visit my clinic.
I always start with the deepest and most obvious acne scars which are the most visual and eye-catching. Hence, I build the skin from the ground up. Since most patients have a variety of acne scar types, I use a variety of methods. For tethered and anchored acne scars, I typically use subcision to untether the fibrous strands. Once I untether the fibrous strands within the scar with a Nokor needle, the acne scar is immediately released and the acne scar elevates. Hence, subcision gives immediate improvement.
For deep ice pick scars, I typically use a TCA cross technique to break down the scar tissue, denature the collagens and stimulate the tissue to start remodeling and raise the scar to a certain depth.
When I have raised all the deep acne scars to a certain depth, I start improving the overall skin texture and the more superficial acne scars with methods such as fractionated laser resurfacing. The fractional laser delivers precise microbeams of laser light into the lower layers of the skin, creating deep, narrow columns of tissue coagulation. This controlled tissue damage stimulates a natural healing process that results in remodeling of the acne scars, creating new collagens, which replaces the tissue loss in atrophic acne scars.
I might also use other methods, including other types of chemical peels, punch excisions, dermal fillers, and skin surgery. This all depends on the types of acne scars, severity and skin type. Please note that my approach is unique in each individual case to achieve the highest possible cure rate in each individual patient.

What is the best treatment for acne scars?
Treating acne scars depends on the type of acne scars, the severity of the scars and the patient’s skin type. The key to success is to analyze each individual acne scar, identify the acne scar type and the skin type and thereafter match the acne scar type with the right method.
Hence, there are no method that is right for all acne scar types. This is an individualized approach. Thus, the acne scar revision program which I plan is always tailored to each individual patient’s acne scars and skin type.

Dr. Ulrik Knap about early acne treatment & acne scarring
The first and most important step in preventing acne scarring is to treat acne as early as possible with the right means. Patients who are prone to develop acne scarring should be treated early on with the best and most effective medication possible, including isotretinoin.
If acne scarring has already developed, the next step is to treat the acne scars with the right methods.
Treating acne scars is a medical art that requires experience and great medical skills. Not one method fits all acne scar types.
I treat acne scars with different methods, and I choose the best methods for each individual acne scar. Combining different methods – when relevant – is the only way to achieve the highest cure rate.
Tailoring an individual acne scar revision program is the key to my success as a laser and acne scar specialist, and one of the reasons why patients come from most of the world to visit my office and have their acne scars treated by me personally.
Best Regards
Ulrik Knap, MD., Laser & Acne scar specialist